:max_bytes(150000):strip_icc()/groinpainfinal-01-5c05dbbdc9e77c00011054d4.png) Groin Pain: Causes, Treatment, and When to See a Doctor
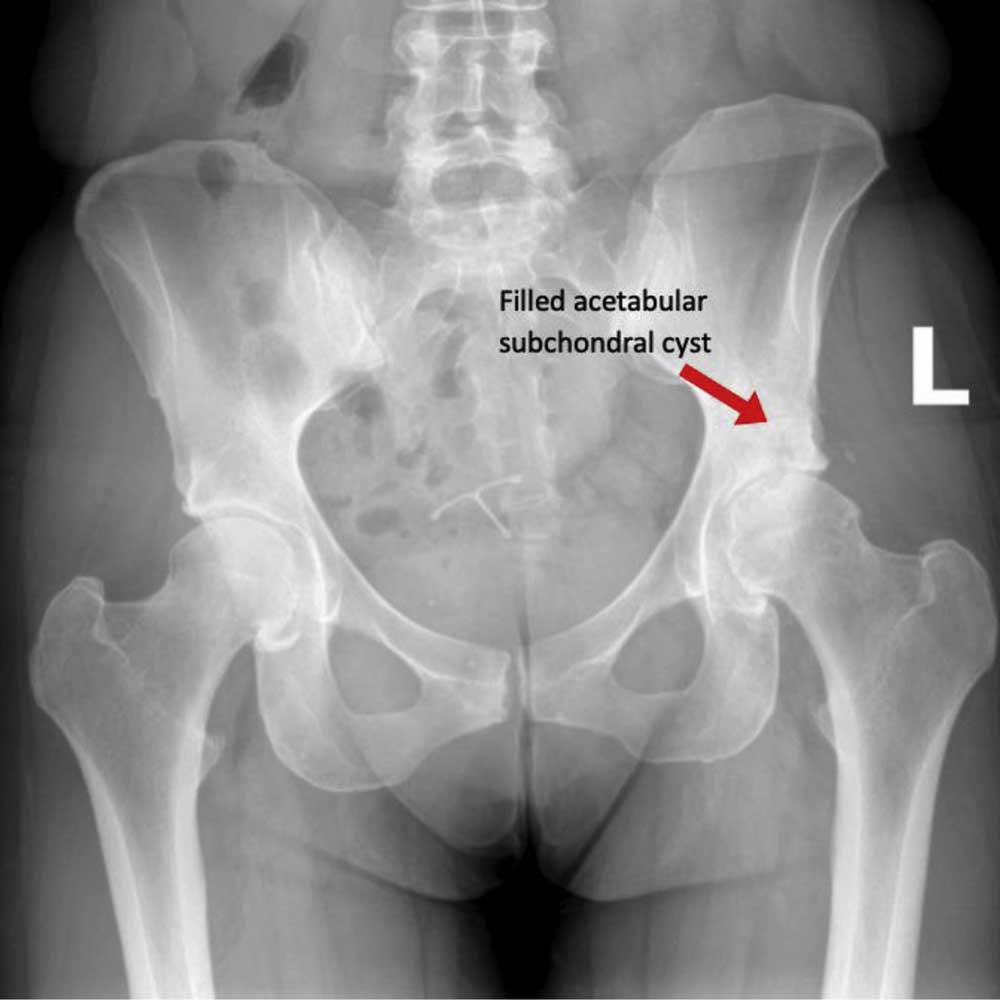
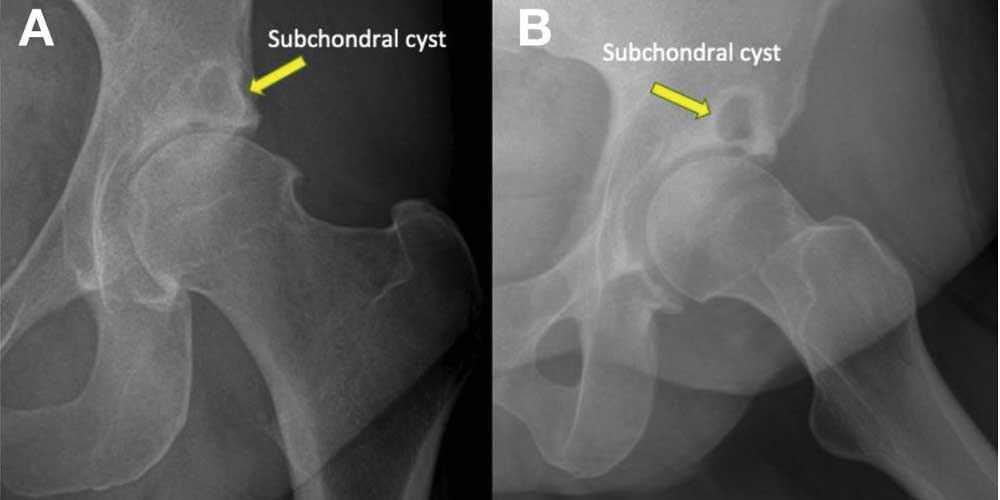
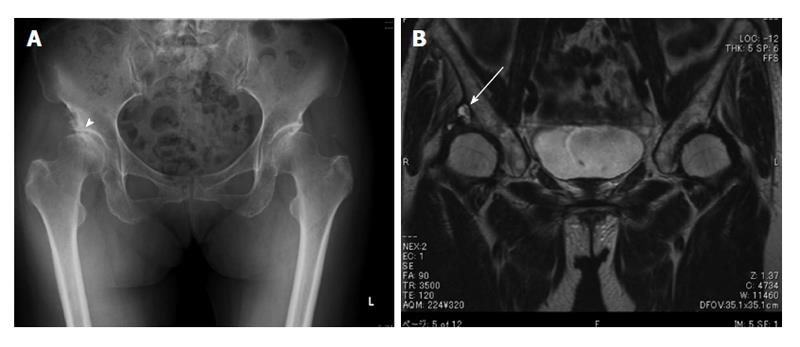
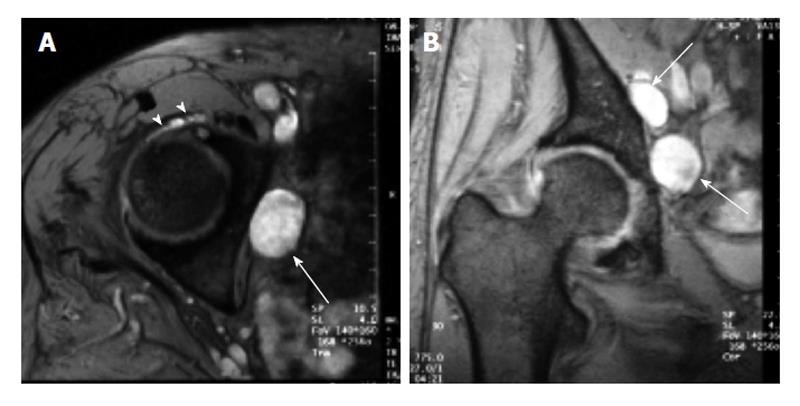
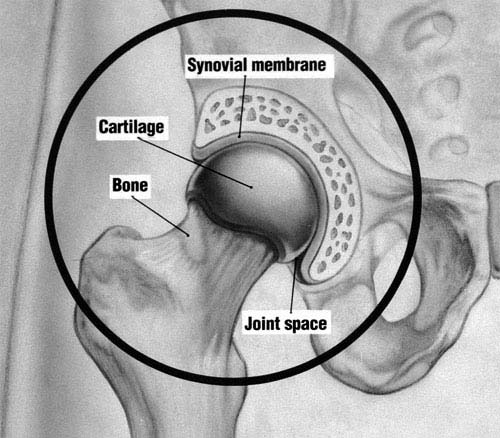
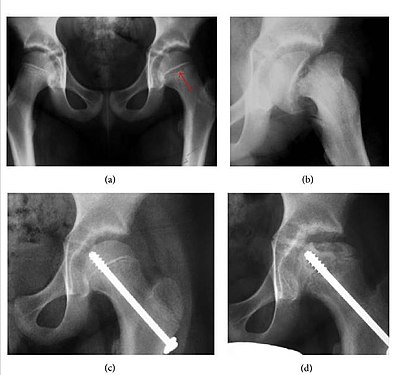
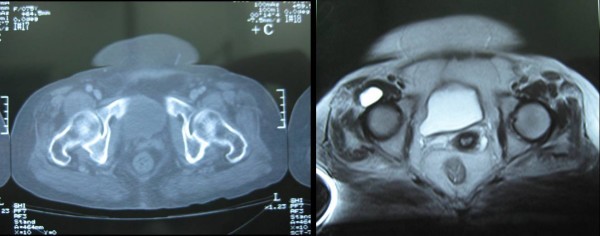
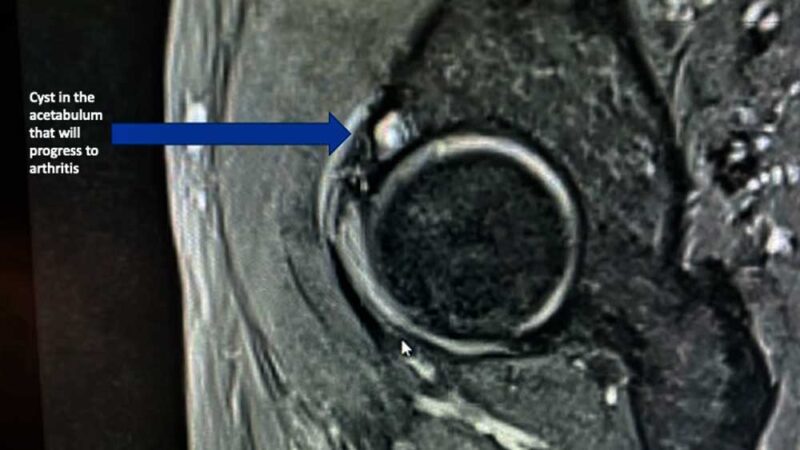
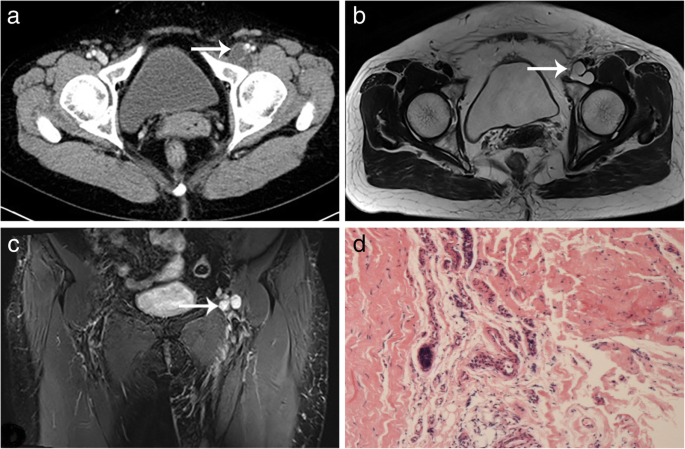
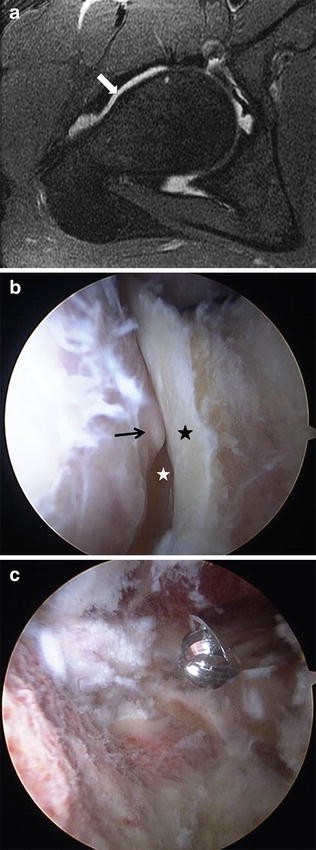
Groin Pain: Causes, Treatment, and When to See a DoctorWarning: The NCBI website requires JavaScript to operate. Cystic lesions around the hip joint Correspondence to: Kiminori Yukata, MD, PhD, Department of Orthopedic Surgery, Hamawaki Hospital Ortopaedic, 4-6-6 Otemachi Naka-ku, Hiroshima 730-0051, Japan. Phone: +81-82-2401166 Fax: +81-82-2401122AstractThis article presents a narrative review of the sections Cy Radiological examination, prevalence, pathogenesis, symptoms and treatment. Cystic lesions around the hip are usually asymptomatic but can be observed incidentally in imaging, such as computed tomography and magnetic resonance. Some cysts may be expanded due to various pathological factors, such as trauma, osteoarthritis, rheumatoid arthritis, or total hip arthroplasty (THA), and may become symptomatic due to the compression of surrounding structures, including femoral nerves, shutters, or sciatica, external iliac intestines or common femoral aspiration, fetrical or external resting vein In addition, when these cysts are associated with osteoarthritis, rheumatoid arthritis and THA, primary THA surgery or revision will be necessary concurrent with cyst excision. The knowledge of the characteristic clinical appearance of the cystic masses around the hip will be useful in determining specific diagnoses and treatments. Basic tip: The aim of this document is to review the clinical characteristics of cystic lesions around the hip joint. Computed tomography and magnetic resonance imaging are useful modalities for the detection of cystic lesions, but it is difficult to distinguish pathological differences between nodes cysts and synovial cysts, including burial. Although cysts around the hip are generally asymptomatic, enlargement of these cysts can cause pain and/or compression of surrounding structures, such as nerves and vessels. The treatment of these cysts depends on its size, the severity of the symptoms and the nature of the underlying disease. INTRODUCTION Cystic lesions can occur around any of the joints or tendon pods in the body. The common locations of the cyst include the wrist, hand, foot, ankle and knee, because it could be much easier to identify cysts near the surface of the body. The development of cysts associated with the hip joint is a rare clinical problem, but may be observed by-catch in clinical examinations of inspection or images, such as ultrasound, CT scan, or MRI (MRI)[]. Some researchers have examined the frequency of cysts in the hips of asymptomatic volunteers using MRI. Their results indicated that 5.8%-26.2% of the asymptomatic hips had a cyst around the joint. In general, 15 synovial burials around the hip joint have been commonly imagined, in particular the bursa iliopsoas, which is the largest synvial burial in the body and present bilaterally in 98% of adults[]. In addition, the herniation of the synvice has been suggested in the surrounding tissue, the displacement of the synvice in the embryonic stage, and the degeneration of the connective tissue in an adjacent joint or a pod tendon as much as possible.[,] Historically, there are 2 types of cysts around the joint or tendon: ganglia and synovial cysts. Ganglion cysts are generally believed to be the result of the mixed-omatous degeneration of certain fibrous tissue structures and do not have a sigh cell coating, while the synovial cysts, including burial, have a sigh cell coating and sometimes communicate directly with the adjacent joint. Both the nodes cysts and the synovial cysts contain a similar gelatin fluid that is very viscous secondary to the presence of hyaluronic acid and other mucopolysaccharides or bleeding[]. It is difficult to differentiate these cysts from clinical and radiological examinations or to determine whether cysts communicate with the joint cavity. Consequently, we use mainly the term "cystic or cystic lesion" when it comes to the tomb, synovial cysts and cyst nodes in this review because they have the same radiological appearance. Cystic lesions around the hip are usually asymptomatic but can cause pain and compression of the surrounding nerves, veins and arteries when enlarged. This narrative review article includes 5 main sections: Radiological examination, prevalence, pathogenesis, symptoms and treatment for cystic lesions of the hip joint. For this review, we search for the keywords "hip cyst" or "hip ganglion" or "hip bursa" using PubMed (National Library of Medicine, Bethesda, Maryland, United States) to obtain the articles published until December 2014. 1056 articles of the keyword "hip cyst", 134 of "hip ganglion", and 239 of "hip bursa" were paired, respectively. All the abstracts or articles selected were reviewed by the authors and articles without an English summary that were not published in English were excluded. As a result searched with PubMed, total 151 articles were considered to be relevant for this review. In addition, we added the 140 related articles using the references of the articles, selected by PubMed, and finally collected 291 articles on cystic lesions around the hip. The aim of this article is to provide an overview of the clinical characteristics of cystic lesions around the hip joint. RADIOLOGICAL EXAMINATIONSConventional X-rays are useful for showing underlying hip joint disorders, such as osteoarthritis, rheumatoid arthritis and acetabular dysplasia, but cannot detect cystic lesions[-]. Arthrography or cytography (bisography) can be used to demonstrate location, size and communication with the joint of the cyst hip[,-,-]. However, the communication between cysts and the hip joint cannot be demonstrated when the communication is very narrow or the root has a verification valve mechanism[]. Ultrasonography is a useful and non-invasive image modality to demonstrate the fluid-filled nature of a palpable mass. Cystic lesions may appear as hypoecoic areas in ultrasound examinations[,-]. This modality can be used to guide the aspirations of needles and/or drug injections[,]. On the other hand, ultrasound does not show subtle joint communication sites and has a limited ability to evaluate associated intraarticular abnormalities. Computed tomography is an excellent tool to evaluate the abnormalities of calcified tissues due to its high spatial resolution[,,,,,,,,-]. Cytos have a lower attenuation than muscle attenuation and higher than fat. The polishing improvement can be seen after intravenous contrast management[,]. Similar to ultrasonography, CT can be used to guide the aspiration of cyst needles[,]. MRI is superior to all other imaging modalities to investigate soft tissue abnormalities, particularly to demonstrate the exact location and extent of injuries around the cyst[,-,,,,,,,,,-]. This technique offers superior contrast of soft tissue and multiplanar capabilities and is not invasive. Images can represent round or ovoid cystic masses with low signal intermediate intensities in T1-weight images and high signal in T2-weight images. Detection of cystic lesions is much easier in recovery images of crushed or short tau investment. The MRI with intravenous administration of the contrast agent, Gd-DTPA, in the weighted image T1 can show edge improvement and is more useful to diagnose synovial cysts because the synovial proliferations have rapid and marked increases in signal intensity.[,,,,] However, after injection of contrast agent, the improvement of the cystevia, even for cysts, can not be evident[.] In addition, MRI is very precise in the description of associated joint disorders, such as acetabular labral tears and degenerative or inflammatory changes[]. The MR arthrography can show in detail the relation of an injury to a joint and surrounding structures[]. PREVALENCIAMost reports on cystic lesions around the hip joints have been case reports, but O'Cooner[] stated that the actual incidence is probably greater than that indicated by rare cases in 1933. We found 3 reports on the prevalence of cysts in asymptomatic hips in the MRI. In 1998, Cotten et al[] reported for the first time the appearance of MR of the hip labrum in asymptomatic volunteers. He described that intralabral cysts were observed in three 52 hip labras (5.8%). Recently, other studies have shown a high rate of cysts around the hip. Schmitz et al[] described cystic lesions in 11 of 42 (26.2%) and 9 of 42 (21.4%) asymptomatic hips identified by 2 different radiologists. Register et al[] reported that cysts were identified in 6 of 45 (13%) asymptomatic participants. These results indicate that the detection of cysts around the hip joint is no longer a rare abnormal finding and the increased sensitivity of the MRI has allowed to identify these cysts. PATHOGENESIS There are pathologically some types of cystic lesions, including thieve, synovial cyst and bursa. Ganglion cysts do not have a sigh cell coating probably due to the result of the degeneration of the mixed tissue[]. While the synovial cysts have a sighal cell coating because they can be caused by the hernia of the synovice in the surrounding tissue or the displacement of the synovio in the embryonic stage. However, the exact cause of these cysts remains unknown[,,,,]. Burials are sacks full of fluids lined by the synovial membrane, which usually present and provide a cushion between bones and tendons and/or muscles. At least 15 synovial graves have been described around the hip joint, including trochanteric, iliopsoas, shutter, and ischial bursa[,,,,,,,,-] (Figure ). Bursa iliopsoas is the largest synvial burial burial burial bursa bursa bursa bursa bursa bursa bursa burs are present bilaterally in 98% of adults[] (Figure ). This structure is among the iliofemoral and pubofemoral ligaments, is adjacent to the thinst and most vulnerable part of the previous capsule, and is the most problematic synovial tomb. In a study of cadaver, Chandler found communication between the bursa iliopsoas and the hip joint in only 14.25% (61 of 400) of the adult bodies and in as many as 40% of the hips with osteoarthritis[,]. The iliopsoas bursitis was first reported by Fricke in 1834 according to Finder[]. In 1887, Sprengel also reported a case of bursitis communicating with the hip joint, according to Gatch and Green[]. Thus, cysts that occur in the previous part of the hip may be inflammation and expansion of the bursa iliopsoas itself or herniation of the previous capsule caused by increased intraarticular pressure and an intrinsically weak capsule secondary to the underlying inflammatory or degenerative joint disease[,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,, On the other hand, it is believed that a disdained bursa shutter is formed by the protrusion of the posterior joint of the hip between the ischiofemoral capsular ligament and the orbicularis zone.[] Trochanteric bursa is located on the side side side of the largest trochanter of the femur[-]. An inflamed trochanterica bursa caused by various conditions is causing pain in the lateral hip[,-]. However, it is difficult to distinguish isolated bursitis, pure synovial hernia articular without bureaux involvement, or ganglionist cysts in radiological or clinical examinations. A female of 58 years old with greater trochanteric bursitis. Coronal (A) and axial (B) MRI images with a cyst weight T2 located in the characteristic position of the most left trochanteric bursa (street). A great trocánter. An 81-year-old female with femoral neuropathy caused by neglected bursa iliopsoas. The Axial T2 weight MRI image shows a cystic lesion, which extends earlier to the iliopsous muscle (A). Computed tomography does not demonstrate any communication between cyst (fleight) and right hip (B). Arrowheads: Contrast material. The hip cytes are usually accompanied by the following hip disorders such as trauma, avascular necrosis of the femoral head, osteoarthritis, rheumatoid arthritis and total hip arthroplasty (THA). Surgical capsular release for hip contracture after spinal injuryThe release of soft tissue from the hip is a common procedure for contracting this joint, especially in patients with cerebral palsy or spinal cord injury. Only one case of cyst formation has been reported to be communicated with the hip joint after this procedure.[] Avascular necrosis of the femoral headThe vascular necrosis of the femoral head is one of the pathogenesis of the formation of the synovial hip cyst[,,,,,]. The necrosis and deformity of the femoral head lead to joint synovitis and result in osteoarthritis of the hip. Cohen et al[] reported for the first time iliopsoas bursitis associated with a vascular necrosis of the femoral head in a 34-year-old female receiving steroid therapy for systemic erythematous lupus. Yoon et al[] reported a similar case involving femoral neuropathy. The X-rays of the tail show deformity of the femoral head and narrowing of the joint space, which results in osteoarthritis[,]. TraumaThe acute or chronic trauma and the sports injuries have been mentioned as factors causing the formation of cysts around the hip[,,,-]. O'Conner[] suggested that the trauma given to bursa iliopsoas during intense hip reflection and the extension was the most likely etiological mechanism[]. Displasia del desarrollo Lin et al[] reported a case of a 35-month-old child with a cyst of hips secondary to a tear. It was treated with thermotomy, closed reduction, and a hip spike for hip development dysplasia when I was 14. Labral When cysts around the hip joint are adjacent to the joint capsule and/or the acetabular labrume in the MRI, it has been believed that the cause of these cysts is synovial fluid that is forced through the labral tear through a single-way valve mechanism[]. This type of cyst is radiologically designated as a paralabral or labral cyst[,,,-,]" (Figure ). In 1989, Haller et al[] first described the relationship between a cystic mass adjacent to the acetabulum and a labral tear. They illustrated that the tissue or the synovial fluid can be extruded from the joint through the labral tear and lead to the accumulation of fluid and formation of cysts in adjacent soft tissues as a factor in the pathogenesis of yuxta-acetabular cysts. In 1994, Tirman et al[] determined that a glynoid labral tear on the shoulder was associated with a cystic mass and called the mass a lay cystic cypress. The same group applied the term to similar cysts of the hip joint[]. Schnarkowski et al[] reported that of the 7 labral cysts, 5 were located in the posterosuperior and 2 in the previous one. He described that the labrum's posterosuperior part was the most vulnerable to mechanical stress and an easier place to detach from trauma, which could lead to the formation of cysts[]. In addition, Magee et al[] reported 10 patients who were subjected to surgery for labral cysts and had associated tears of labral in the area of the labral cyst. Seven of the tears occurred later and 3 occurred earlier. Recent reports of the series of cases described that the paralabral cysts were located antero-superiorly in 56% (10 of 18) of the patients, previously in 22% (4 of 18), posterosuperiorly in 17% (3 of 18), anteroinferiorly in 6% (1 of 18), later in 0%, and posteroinferiorly in 0% in arthronic analysis MR[]. This result was consistent with the fact that most tears have occurred antero-superiorly in the evaluation by the arthrography of the MR[,]. The labral cyst of the hip can be a predisposition to the labral pathology. MR arthrography can increase sensitivity and precision for the detection of associated tears. Recently, arthroscopic treatment has been reported for acetabular labral tear and paralabral cyst[,]. Tey et al[] reported a case with acetabular lagrim and labral cyst caused by the impingement of psoas. In this case, the pasoa tendon was released and the labral cyst was excised; readjustment of the tear was finally realized using a suture anchor. Kanauchi et al[] also reported a combination treatment with arthroscopic labral repair and ultrasound-guided cyst aspiration for the paracetabular paralabral cyst that causes femoral nerve paresthesia. In contrast, Lee et al[] described an arthroscopic treatment for cystecnic decompression and debridation of degenerative labrumus for labral cyst and tear. Thus, the arthroscopic findings will be useful for better understanding the labral cysts. A 50-year-old female with right hip pain. The MRI image with Axial T2 weight shows a labral cyst and paralabral (fleight) in the previous aspect of the right hip joint. OsteoarthritisOsteoarthritis is a degenerative joint disease that causes pain and joint stiffness. More than 80% of all cases of idiopathic osteoarthritis of the hip joint can be due to congenital or developmental subtle defects, which increase joint incongruity and concentrate dynamic load (Figure). The dynamic loads cause displacement of synovial fluids, which in turn can cause the development of synovial cyst[,,,,,,,,,,,,,,-].A 70-year-old female with cystic lesion associated with osteoarthritis. The x-ray of the lower pelvis reveals the secondary osteoarthritis of the right hip due to acetabular dysplasia (small head) (A). The T2 coronal magnetic resonance imaging shows a cystic mass (fleight) located above, connected to the right hip joint (B). Rapid destructive osteoarthritis of destructive hipRapidly disease (RDHD) is a rare entity that involves joint destruction of aggressive hips within 6-12 mo of startup. Inflammatory arthritis is always caused by cartilage and bone destruction in such cases. It has also been seen in 2 reported cases of RDHD[,].Reumatoid arthritisReumatoid arthritis is an autoimmune disease that results in a chronic inflammatory response of the synovial joint capsule to inflammation due to excess of synovial fluid and the development of the synovio. The occurrence of the synovial cyst of the hip in patients with rheumatoid arthritis has been reported.[,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,-].Coventry et al[] described 3 cases of rheumatoid synovial cysts of the hip. Two out of 3 patients had edema of the extremities due to the compression of the femoral vein caused by enlarged synovial cysts. They documented 3 theories on the etiology of the formation of rheumatoid synovial cysts. First, overproduction of the synovial fluid in a rheumatoid cyst can increase intraarticular pressure and dissipate the joint capsule. Second, bursa iliopsoas, which sometimes connects directly to the hip joint, may be involved in the rheumatoid process with the formation of excessive amounts of liquid[,]. Thirdly, the necrosis of a subcutaneous periarticular rheumatoid nodule could result in the formation of a yuxtaarticular cyst. However, the exact etiology of rheumatoid synovial cysts cannot be determined. Although some similar cases of rheumatoid cysts have been reported after the Coventry cases[,,], interestingly, all cysts associated with rheumatoid arthritis in the reported cases were previously located. This finding suggests that bursa iliopsoas is involved in cyst formation associated with rheumatoid arthritis. Juvenile idiopathic arthritis Juvenile idiopathic arthritis (JIA) is an autoimmune arthritis in children under the age of 16. Iversen et al[] described the expansion of bursae iliopsoas communicated with the hips in a JIA patient. Polymyalgia rheumaticaPolymyalgia rheumatica (PMR) is an inflammatory disorder that causes pain and stiffness in the neck, shoulder and pelvic circumference. Tani et al[] reported a case of expansion of bursa iliopsoas due to PMR. Hip Artroplasty In 1984, Kolmert et al[] reported for the first time 2 cases of cyst formation after THA. In addition, some cases of cystic lesions have been published after the joint substitution[,,,,,,,,,,,-]. Initially, these cysts were believed to be subclinic infections, but are currently called " granulomatous pseudotumor" resulting from polyethylene, metal, or cement debris, which is phagocytes by inflammatory and macrophages cells that cause a foreign bodily reaction[,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,] (Figure). On the other hand, some cysts can be distended iliopsoas bursitis as a tissue response to use rubble, but not the newly formed granuloma[,,,,,,,,,,]. A 76-year-old male with pseudotumor after the total cemented hip arthroplasty, implanted 18 years earlier. The image of the magnetic resonance of the short coronal investment of tau shows a cystic lesion (fleight) adjacent to the acetabular component (small head). In 2005, Willert et al[] described for the first time the development of an inflammatory synovial reaction as a novel complication associated with replacements of metal hips[,]. A different histologic pattern is observed and is characterized by diffuse perivascular infiltrates of T and B lymphocytes, high endothelial venulos, exudation of fibrines, eosinophiles and necrosis. It is believed to be a variation of type IV delayed hypersensitivity and has been called an lesion associated with vasculitis dominated by septic lymphocytes (ALVAL). Adverse reactions to metal debris, including ALVAL and pseudotumor formation, should be considered as a diagnosis in any patient with inexplicable pain of the groin or a mass after a M TEMA[,,,,,,,-]. Generally, patients with pseudotumors may be asymptomatic[,] or present with mild pain of the groin[,,] intestine. Cystic lesions associated with THA can be one of the signals for implant failure or loosening. Other cysts containing hip gas have been reported infrequently. The gas can be seen in conventional x-ray, linear tomography or CT[]. This gas can be difficult to differentiate from excessive intestinal gas and other causes of gas within soft tissues.[] The gas can be present within unserved bursae iliopsoas due to a gas pumping mechanism, which can lead to a misdiagnosis. Silver et al[] reported 3 cases of nodes containing gas that are derived from hip joints with advanced osteoarthritis. Haller et al[] also reported that the gas was shown in 4 cystic lesions around the hip joint associated with the degenerative hip disease. It should be noted that a cystic mass around the hip may not be a synovial cyst or node, but may originate from the advent of the common femoral artery or vein. The latter has been called "aventicial cystic disease", which is a rare type of disease of non-atherosclerotic peripheral vessels and is characterized by the accumulation of a mucinic substance in adventitia[-]. These substances cause symptoms of intermittent claudication or swelling of the legs due to obstruction of the arteries or veins. The differential diagnosis of a mass in the inguinal region includes various conditions, such as the pigmented villonodular synovitis[,], synvial condromatosis[,,], arterial aneurysms, femoral hernias[,], inguinal lymphadenopathy and abscess[,,,,,,,,,,,,,] (Figure ). Careful clinical and radiological tests will help confirm or exclude a diagnosis. A 93-year-old male with hemiartroplasty infection for the left femoral neck fracture. The image with axial T2 weight reveals a cystic lesion with a fluid-fluid level (small) adjacent to the posterior aspect of endoprossis (small head). SYMPTOMSThe cysts around the hip joint are often asymptomatic[,] (Figure ). When cysts prevent nerves or vessels, they can become symptomatic. A 71-year-old female with left femoral neck fracture. The T2 coronal magnetic resonance imaging shows a multi-locular asymptomatic cystic mass (fleight), which communicates with the right hip joint. Pain and/or swelling Although pain is not a universal characteristic, it is often the earliest and can be the only cyst symptom, which may include bursitis[-,-,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,-]. Inguinal mass and pain in the groin or thigh usually include clinical presentation in some patients. Akman et al[] reported a case of a hip node that had symptoms of right-sided English pain. A larger mass caused nocturnal femoral pain[]. Inguinal inflammation has also been reported as another rare presentation of a hip cyst when cysts grow earlier[,,,] or later[]. A soft mass on the femoral triangle could be misdiagnosed as a femoral hernia[,].SnappingIliopsoas bursitis is often associated with the hip syndrome that sprouts[,,,]. The hip syndrome that breaks with the iliopsoas tendon over the iliopectineal eminence and the previous hip capsule or a lower trochanteric bony prominence. Harper et al[] reported 2 cases with a painful audible hip. In the literature, snapping was reproduced voluntarily by extending the flexed hip, kidnapped and rotated externally, and the iliopsoas bursography was a useful technique for the diagnosis of this syndrome. The hook could disappear by release of the tendentious portion in these cases.[,] Peripheral nervous breakdownFemoral awakening: Approximately 20 cases of femoral nervous compression due to a cystic lesion around the hip joint have been described in the literature[,,,,,,,,,,,,,,,,,,,,,,-]. Symptoms were described as root pain caused by the compression of the femoral nerve and by hypoesthesia and/or paraesthesia in the groin radiating towards the mid thigh, the anterior aspect of the knee, and the medial side of the leg and the lower foot. Some patients complained of their inability to climb stairs and walk due to hip pain and muscle weakness. These symptoms mimic L2-4 radiculopathy with lumbar disorders, such as hernia of the lumbar disc and lumbar spinal canal stenosis[,]. The physical exam can reveal sensitivity over the previous hip, limited range of movement of the affected hip joint, sensory alteration of the femoral nerve zone and thigh atrophy. The iliopsoas and gnamor muscle quadriceceps may be weak[,] accompanied by reflections of decreased patellar tendon[,]. The hip stays in bending with some adduction and external rotation. Pain is caused by hyperextension, abduction or internal rotation of the hip. In radiological examinations, the X-ray of the pelvis can show a severe degenerative hip disease, which causes iliopsous bursitis in some cases[,,,,,,,]. The cysts with femoral nerve compression are always located on the previous hip and are mostly synovial cysts due to the relationship with bursa iliopsoas (Figure). On the other hand, although rare, some cases have been reported with femoral nerve compression caused by ganglion cyst[,]. Recently, some reports have described THA wastes that produced a clinically detectable mass that could cause delay in femoral nerve paralysis[,,,,], although some cases had solid pseudotumors but not cystic lesions. Locking nerve: Obturating neuropathy can be caused by several conditions, such as pelvic fracture, THA or hernia, but the nervous compression shuttered by a cyst is extremely rare. Only 4 cases have been reported.[,] In 2002, Campeas et al[] reported for the first time a case with obturating neuropathy caused by a ganglion cyst that emerged from the hip joint. In 2005, Yukata et al[] presented a case with obturating neuropathy caused by a cyst associated with an earlier acetabular labral tear and its detailed findings of MRI. Stuplich et al[] also reported a case with femoral and obstructive neuropathy combined with a synovial cyst of moderate hip osteoarthritis. The main symptom of obturating nervous compression is pain in the right groin and anteromedial thigh[]. The tenderness occurs on the muscles of the driver, and the sign of Patrick (hyp flexion, rapture, external rotation, extension position) can be positive and passive examination of the elevation of the straight leg is negative. The weakness of the hip aductors due to pain and the absence of the reflex of the aductor could have been detected.[] The magnetic resonance of the pelvis has shown a cystic lesion in the media aspect of the right acetabulum with its stem continuing to the previous labral tear[] or extending to the obstructing muscles to the obstructing nerve[] (Figure ). In addition, the muscles of the clotting nervous zone can show atrophy and increased signal intensity in T2 sled images, indicating denervation[,]. A 75-year-old female with obturating neuropathy. Axial (A) and coronal (B) recovery of tau investment short magnetic resonance imaging show that the location of the cystic masses (fleets) is consistent with the shutter nerve site (Ref: [26]). The stem of the cyst was connected to the previous joint capsule (small heads). Cyatic nerve: Cyatic neuropathy has been reported secondary to a cystic lesion around the hip joint[,,,-]. In 1991, Juglard et al[] reported for the first time a case with cystic nerve compression due to a cystic lesion. In addition, some similar cases have been reported until 2014[,-,]. These patients had an increasing pain of buttocks that radiated downwards into the back thigh and knee and the side aspect of the lower leg and sole, which is the ciatic call. The patient may have a side calf and sole paresthesia. The physical exam can reveal any sensory disturbance or muscle weakness of the lower leg, and the hip range of the movement is either complete or slightly limited. The disease may be on the back hip. The straight leg elevation test was negative in all reported cases, but the pain around the hip was caused by hip rotations[,]. The magnetic resonance clearly showed a cystic mass in the sciatic musca or later extended to the intertrocárica lesion of the femur. The histologic evaluation of these cysts showed that the cyst wall was composed of variantly dense fibro-conexive tissue without lining cells, suggesting a cyst node[,,,], while the recent case reported by Salunke et al[] was histologicly diagnosed as a synovial cyst. Cyatic neuropathy as late complication is sometimes caused by cystic formation due to polyethylene or titanium carry debris after THA[,]. Fischer et al[] first described a patient with cyatic neuropathy following the compression caused by an intrapelvic synovial cyst formed in response to debris wear. Crawford et al[] reported 3 cases of cyatic nerve compression caused by polyethylene debris wear in THA screening surgery. Recently, Mert et al[] also reported that the use of lower polyethylene on the edge of the coating and crack of the titanium acetabular shell was observed in the THA review. The histologic examination showed that the drying cyst included giant cells of the foreign body along with abundant deposits of titanium and polyethylene particles. These cystic masses with cyatic neuropathy after THA appear to be synovial cysts connected with the joint space. We present findings of MRI of an unprecedented case of cyatic neuropathy due to a cystic lesion in which the patient had a 1-mo history of increased pain in the left buttock and lower leg with an insidious beginning (Figure ). A 67-year-old female with a sciatica. The image of the magnetic resonance of the short axial tau investment shows cysts in the back aspect of the left acetubulum (spots). The stem is connected to the posterior joint capsule (small head). Side femoral nerve: Paraesthetic Meralgia is numbness or pain in the outer thigh caused by the intromission of the lateral femoral nerve cutaneous. Only one case was reported as a compression neuropathy caused by a hip joint cyst associated with rheumatoid arthritis[]. Blood CompressionThe compression of the femoral artery causes ischemia of the leg. Byström et al[] reported a 75-year-old female with a large cyst that compresses the femoral artery. Symptoms were an intermittent and unpleasant feeling of coldness in the foot and hip pain. The cyst was communicated with a severe osteoartrist hip joint. Beardsmore et al[] and Stanek et al[] also reported ganglion cysts that emerged from the hip joint or psoas that compressed the artery and caused symptoms of intermittent claudication. In addition, Zack et al[] presented an occlusion of the external illic artery due to a giant synovial cyst that was produced by polyethylene debris wear after THA. In such cases, angiography can demonstrate occlusion of the common external or femoral artery[,].Venous ComparisonThe compression of the femoral or ilic vein caused by a cyst of the hip joint results in the swelling of the legs, which resembles the cause of the deep vein thrombosis, and is called pseudotrombophlebitis. Previously, more than 40 cases of venous compression due to a cystic lesion around the hip have been described in the literature[,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,-]. The x-ray of the pelvis was useful to observe the presence of hip disorders because rheumatoid arthritis or osteoarthritis was present in about two thirds. The extrinsic compression of the external delusional veins and femorals by the mass can be observed by the venography. Venography is also useful if deep vein thrombosis is suspected and needs to be excluded. A cystic lesion of the hip joint should be taken into account in the differential diagnosis of deep vein thrombosis. Urinary symptoms When a cyst compresses the ureter or bladder, the patient may complain of dissuria, frequency, and nocturia, or have no symptoms.[,,] Intravenous skin may reveal the obstruction of the ureter, which results in kidney hydronephrosis.[] Watson and Ochsner reported a case with high urinary frequency and drip caused by the compression of the side walls of the bladder due to a neglected bursa iliopsoas[]. TREATMENTAlthough variable therapeutic strategies have been used for cystic lesions of the hip, the treatment of cysts depends on its size, the severity of symptoms, the nature of the underlying disease or the associated condition, and the presence or absence of local compression. When hip cysts are asymptomatic, they can be treated by observation[,]. When an enlarged and painful cyst is suspected to be a synovial cyst or bursitis, rest, non-steroidal anti-inflammatory drugs, local heat application and physical therapy can provide symptomatic relief.[,,,,] If the cyst is a synovial cyst caused by rheumatoid arthritis, prednisone and metotrexate can be effective in reducing symptoms,[] In addition, injection of local anesthesia and/or corticosteroids after needle aspiration may be considered as a treatment option[,,,,,,,,,]. When patients have compression neuropathy or obstruction of an artery, vein or ureter due to a cyst, they are often treated by aspiration of the cyst or surgical excision. Colasanti et al[] reviewed 27 cases with compression of ships due to cysts. The aspiration of the needle was initially performed in 8 patients, and the other 19 patients were treated by surgical removal of cysts associated with synvectomy or capsulectomy[,,,,,,,,,,,,,,,,,,,,,,,,,-,-,]. Inflammation of the lower extremity was repeated in 3 of 8 patients (37%) initially treated with needle aspiration, while recurrence was observed in only 1 patient with surgical treatment (5%). This result indicated that surgical excision is a more reliable technique for the prevention of recurrence[,,,,,]. However, we still believe that the aspiration/point of needle should be the first treatment option because it has been shown that the simple aspiration/point of needles decreases the size of the cyst and the symptoms in some cases involving venous or nervous compression[,,,,], is easier to perform and less invasive than surgery, and the content of a cyst can help the diagnosis[,]. When a cystic lesion associated with osteoarthritis, rheumatoid arthritis and THA is excised, primary THA surgery or review may be necessary to relieve pain and improve hip functions[,,,,]. CONCLUSION Almost all cystic lesions around the hip joint will be asymptomatic, but recently they are frequently discovered by CT or MRI examinations. The expansion of a cyst, including the bursa, could cause unexplained hip pain. In addition, when cysts compress their surrounding structures, such as nerves or vessels, several symptoms will appear depending on the compressed tissue. In orthopedics, leg pain, intermittent claudication or leg edema are common symptoms in the lumbar spine or vascular disorders. In such cases, cysts around the hip should be regarded as the differential diagnosis. FootnotesP- Reviewer: Musumeci G, Ohishi T S- Editor: Ji FF L- Editor: A E- Publisher: Liu SQConflict-of-interest statement: All authors claim they have no conflicts of interest. Open-Access: This article is an open access article that was selected by an internal editor and reviewed by external experts. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0), which allows others to distribute, remix, adapt, build on this non-commercial work, and license its derivative works in different terms, provided that the original work is properly cited and the use is not commercial. See: http://creativecommons.org/licenses/by-nc/4.0/Peer-review initiated: April 24, 2015 First decision: June 9, 2015Press article: September 8, 2015ReferencesFormats:Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
Identify and treat your Groin and Hip PainYour groin is the area where the upper thigh and lower abdomen are found. Your hip joint is on the same line below your groin. Because the former, or the forehead, of your hip and your groin are approximately in the same area, English pain and previous hip pain often happen together. Sometimes pain begins in one part of your body and spreads to another. This is called radiant pain. It may be difficult to say what is causing pain in the English and hips because the pain of a problem in the hip often radiates into your groin, and vice versa. We will review the many possible causes of pain of the English and the hip, which you can do for them, in addition to a section on home treatments for common problems involving muscles and bones in that area. Pain or radiating from your inside and hip area can be sharp or boring, and can suddenly start or accumulate over time. Pain of your muscles, bones, tendons and usually increases when you move. The type and severity of the pain in the hip and the English varies depending on the cause. The pain characteristics and symptoms associated with specific causes are listed below along with common treatment options. Avascular necrosis (Osteonecrosis) occurs when the upper part of the femur does not have enough blood, so the bones die. The dead bone is weak and can easily break. Symptoms of avascular necrosis This causes a thorn or pain in the hip and the groin. Pain is severe and constant, but it worsens with position or movement. Treatment of Avascular Necrosis When avascular necrosis affects the hip, it is usually treated with hip replacement surgery. When avascular necrosis affects the hip, it is usually treated with hip replacement surgery. Bursitis is the inflammation of the fluid-filled sac, called a bursa, on the outside of its hip. Bursae reduces friction between the tendon and the underlying bone. This is usually an excessive injury. The bursa is irritated due to repetitive movements, which causes pain. Symptoms of Bursitis Neuroitis is an acute pain that worsens with movement, prolonged position or when it is on the affected side. Pain can be severe. Femoroacetabular Impingment In this condition, the two bones of the hip joint come in abnormally close contact, which can pinch the soft tissue or irritate the joint, causing pain. It can be caused by abnormal bone development when you are young.Femoroacetabular impingence Symptoms Pain gets worse after sitting for a long time, standing for a long time and with movements like getting out of a car. Pain can limit how much you can move your hip. Hip Fraction A rupture at the top of the femur can occur if you hit very hard, from a fall, or when the bone is destroyed by the cancer. If you have osteoporosis, your bones are weaker and have a greater risk of rupture. Osteoporosis and occurs most often in older women. Symptoms of hip fracture Breaking a hip bone can be very painful. It gets worse when you try to move your leg or bear weight with it. Hip Fracture Treatment This is a medical emergency and may require surgery to repair or replace the hip. You will usually need long-term physical therapy after surgery. This is a medical emergency and may require surgery to repair or replace the hip. You will usually need long-term physical therapy after surgery. Labral The labrum is circular cartilage that surrounds your hip shot. It can tear due to trauma, excessive injury or femoroacetabular impingence. Labral tear symptoms Pain can be boring or acute and increases with activity, weight gain, and when it straightens the leg. You can feel clicks, pops, or captures in your joint, and you may feel weak, as you will. Labral Lagrim Treatment You can start with conservative treatment, including physical therapy, rest and anti-inflammatory drugs. If this fails, you may need arthroscopic surgery to permanently repair the broken labrum. You can start with conservative treatment, including physical therapy, rest, and anti-inflammatory drugs. If this fails, you may need arthroscopic surgery to permanently repair the broken labrum. Osteoarthritis Aging, cartilage — which helps the bones in a joint move smoothly — is worn out. This can lead to , which causes painful inflammation in the joint. Symptoms of osteoarthritis This causes constant pain and stiffness in the joint of the hip and the groin. You can feel or hear grinding or click on your hip. Pain improves with rest and worsens with movement and position. Treatment of osteoarthritis pain is initially treated conservatively with and physiotherapy. Weight loss helps if you are overweight. When you progress and start causing severe pain and trouble walking or doing daily activities, you may need to. It is initially treated conservatively with and physiotherapy. Weight loss helps if you are overweight. When you progress and start causing severe pain and trouble walking or doing daily activities, you may need to. Stress fracture A occurs when the bones in the hip joint gradually weaken from the repetitive movement, such as running. If not diagnosed, it eventually becomes a true fracture. Symptoms of stress fracture Pain increases with activity and weight. It can be so serious that you can no longer do the activity that caused it. Stress Fracture Treatment You can test home treatments for symptomatic pain relief and inflammation. If you do not get better or pain is severe, it is important to see your doctor before developing a true hip fracture. Your doctor will determine whether the bone will heal with long-term rest or if you need another treatment as a surgical repair to permanently correct the problem. You can try home treatments for symptomatic pain relief and inflammation. If you do not get better or pain is severe, it is important to see your doctor before developing a true hip fracture. Your doctor will determine whether the bone will heal with long-term rest or if you need another treatment as a surgical repair to permanently correct the problem. The narrow groin occurs when any of the English muscles connect the pelvis to their injury by stretching or breaking. This causes inflammation and pain. It often happens due to overtraining or while playing sports, usually while running or changing direction, or moving your hip with clumsyness. A can be mild or severe depending on how much muscle is involved and how much strength is lost. About Muscle Tension PainThe pain caused by muscle tension gets worse with movement, especially when: Pain comes suddenly. Muscle spasms can happen. You may notice bruising or swelling in your groin and upper thigh. The range of motion of your hip can be reduced, and your leg may feel weak. You might have trouble stopping or walking through the pain. Tendonitis is when a tendon, which connects the muscle to the bones, is inflamed by overuse of the muscle. Because tendons are attached to the bone in the hip and muscle in the groin, the pain can also start on your hip and radiate your groin. About tendonitis pain Pain has a gradual beginning. It gets worse with activity and improves with rest. The pain of organs and tissues that are not part of the usually does not increase with the movement, but can worsen with other things, such as its menstrual cycle. This is especially true if you have endometriosis or ovarian cysts. Endometriosis is a condition in which the tissue that normally covers the uterus, called endometrial, grows somewhere outside the uterus. It usually grows in an organ in the pelvis. When it grows near the hip or the groin, it can cause pain in these areas. About endometriosis pain The pain begins where endometriosis is found and can be radiated to your hip and groin. The intensity usually cycles along with its period. Other symptoms include heavy menstrual bleeding and abdominal cramps. Endometriosis TreatmentEndometriosis is usually given with medications or .Endometriosis is usually given with medications or .Ovarian cyst is fluid-filled sacs that grow in ovaries. They are common and usually have no symptoms. When symptoms may cause pain, sometimes severe, that may be radiated to the hip and the groin. About Ovarian cyst pain This usually causes pain in the lower pelvis of the side with the cyst. Pain can be radiated to the hip and the groin. Other symptoms include feeling full and swollen. Pain can be worse during menstruation. Ovarian cyst treatmentOvarian cysts can be treated with, which prevents them from forming. Cysts that are large, very painful or causing other problems can be eliminated with . Ovarian cysts can be treated with , which prevents them from forming. Cysts that are large, very painful or causing other problems can be eliminated with . Less common causes of simultaneous pain of the hip and the groin include: Mild to moderate musculoskeletal lesions, such as muscle tension, bursitis, femoroacetabular imping and tendonitis, can be generally treated at home. By reducing inflammation, you can temporarily improve symptoms and often cure the condition. Possible treatments include: If you are not improving or your symptoms are severe or worse, you should consult your doctor for diagnosis and treatment. Sometimes your doctor may suggest an injection to reduce inflammation or, for severe tears and injuries, arthroscopic surgery to permanently repair the problem. Physical therapy helps improve the symptoms of most musculoskeletal conditions. It is also used to strengthen your muscles and improve the movement range of the hip joint. You can show exercises you can do at home. When you have pain from the groin and hip, the most important thing your doctor does is to determine what you are causing. Because many structures in the area of your groin and hip and symptoms can be similar, this can be difficult unless there is an obvious cause, such as a broken hip. A correct diagnosis is essential to determine the proper treatment. Your doctor may ask: Your age is useful because some things are more common in certain age groups. For example, osteoarthritis and fractures are more common in older people. Problems in soft tissues, such as muscle, bursa and tendons, are more common in people who are younger and more active. Tests for the pain of the groin and hip A test will usually include the feeling of the exact location of your pain, moving your leg in several ways to reproduce the pain, and test your strength by having to resist when you try to move your leg. Sometimes your doctor needs more information and you will get an image study, such as:Artrocopy, where a light tube is inserted with a camera through the skin on the hip, can be used to look inside your hip. It can also be used to repair some hip problems. Most of the time, the pain in the hip and the groin is caused by a problem with the hip bones or other structures in or around the hip joint. Muscle tension is another common cause. Occasionally it is caused by pain by radiating something near the hip and the groin. Determining the cause of hip and English pain can be very difficult. If your symptoms are severe or your pain does not improve with home treatment, you should consult your doctor to get accurate diagnosis and proper treatment for you ingle and hip pain. When treated correctly and quickly, most people with hip and English pain have a good result. Read this now.
Hip Cysts | Acetabular Paralabral Cyst & Subchondral Cyst | FAI | Manhattan, New York City, NY
An unusual cause of pain in both hips | Annals of the Rheumatic Diseases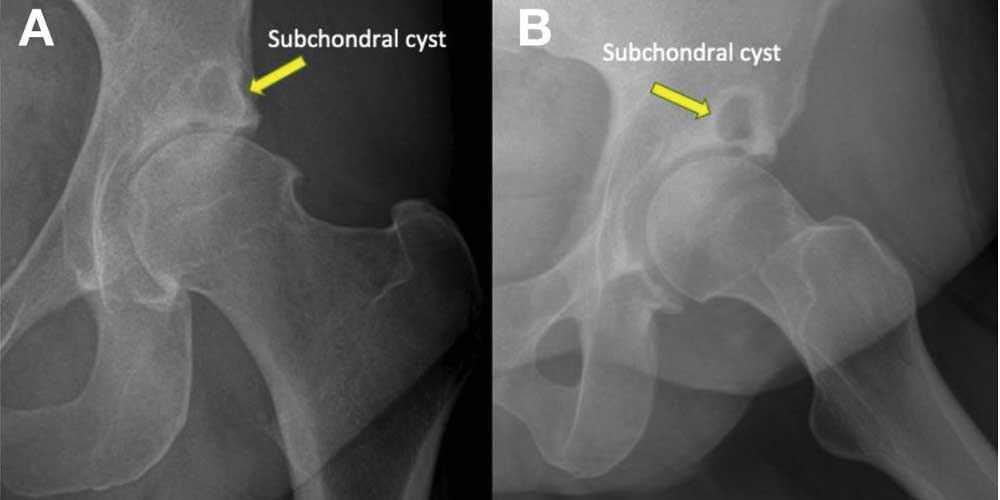
Hip Cysts | Acetabular Paralabral Cyst & Subchondral Cyst | FAI | Manhattan, New York City, NY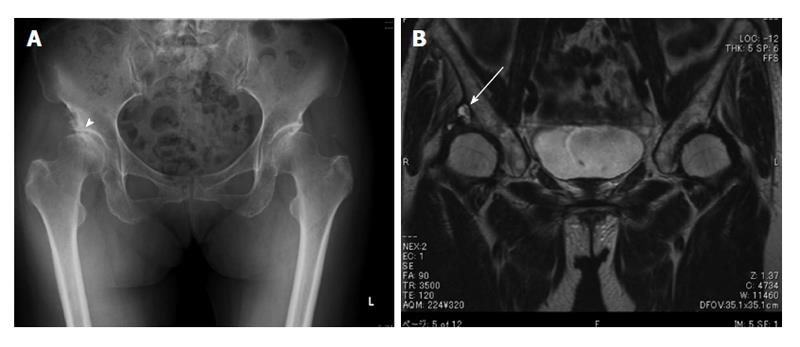
Cystic lesion around the hip joint
Cystic lesion around the hip joint
A 24-year-old woman with right groin pain
A 40-Year-Old Man with Increasing Hip Pain - JBJS Image Quiz
Hip And Groin Pain Worse When Sitting - Can Ovarian Cysts Cause Back And Hip Pain
A 40-Year-Old Man with Increasing Hip Pain - JBJS Image Quiz
Hip Arthritis (Osteoarthritis): Orthopaedic Associates:
Treatments for Groin Pain in Women – Caring Medical Florida
Unilateral Leg Swelling Caused by Common Femoral Vein Compression by a Hip Ganglion Cyst in the Groin - ScienceDirect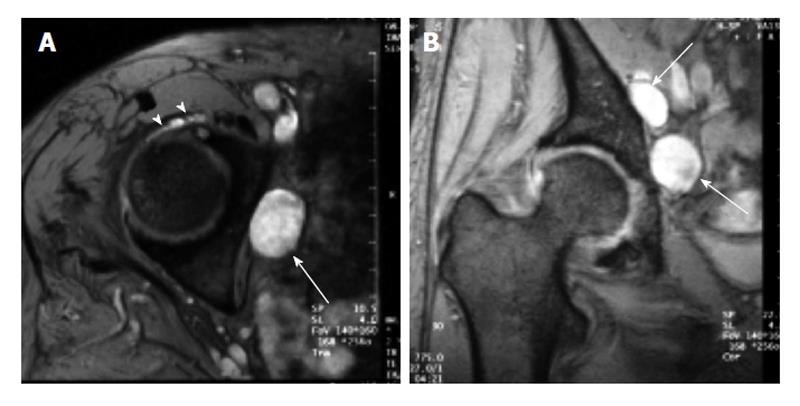
Cystic lesion around the hip joint
A 48-Year-Old Woman with Intermittent Groin Pain - JBJS Image Quiz
Managing hip pain in athletes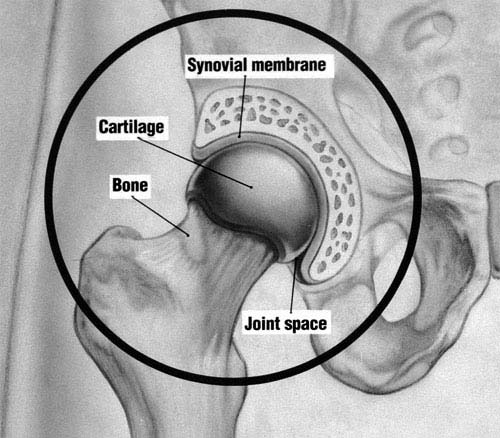
Osteoarthritis of the Hip (Hip Arthritis) | UW Orthopaedics and Sports Medicine, Seattle
Alternatives to hip replacement: The evidence for non-surgical treatments – Caring Medical Florida
Hip Osteoarthritis - Symptoms, Causes, & Treatment - BoneSmart.org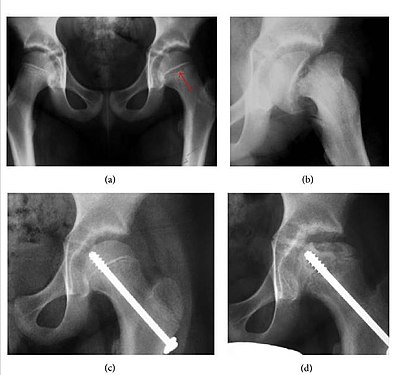
Hip pain - Wikipedia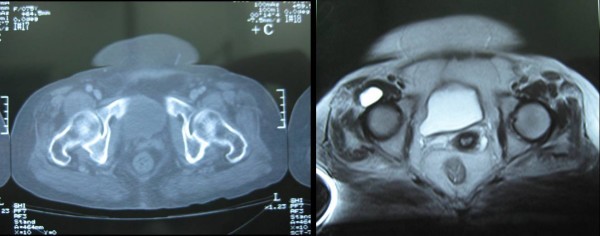
Femoral nerve compression secondary to a ganglion cyst arising from a hip joint: a case report and review of the literature | Journal of Medical Case Reports | Full Text
A 48-Year-Old Woman with Intermittent Groin Pain - JBJS Image Quiz
Osteoarthritis of the Hip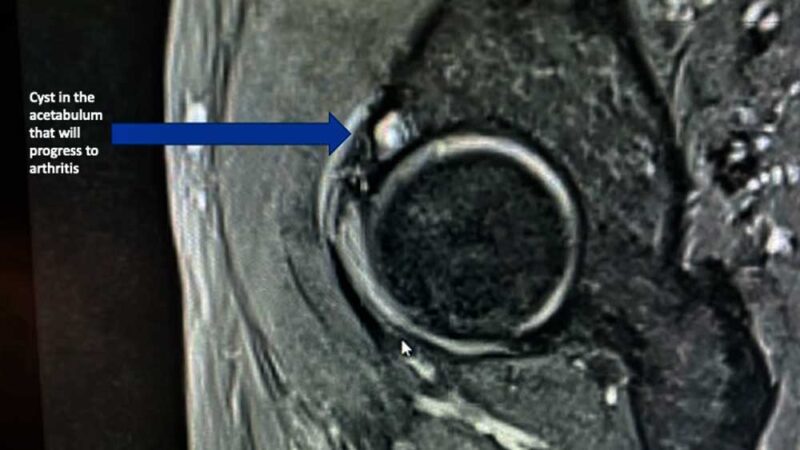
Hip Cysts | Acetabular Paralabral Cyst & Subchondral Cyst | FAI | Manhattan, New York City, NY
Alternatives to hip replacement: The evidence for non-surgical treatments – Caring Medical Florida
A 24-year-old woman with right groin pain
An Unusual Case of Synovial Cyst of the Hip Joint Presenting as Femoral Vein Compression and Severe Lower Limb Edema - ScienceDirect
Paralabral cysts. (a) Sagittal proton-density-weighted fat-suppressed... | Download Scientific Diagram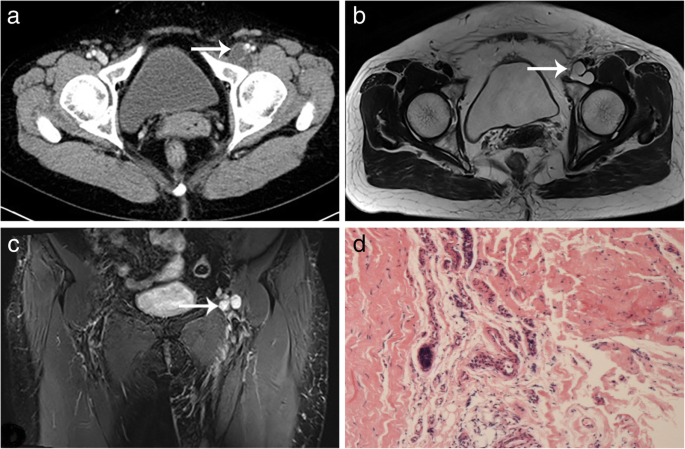
Synovial cysts of the hip joint: a single-center experience | BMC Surgery | Full Text
Hip Ultrasound Scan
What is a Hip Cyst? (with pictures)
Physiotherapy Treatment for Groin Pain - BENPHYSIO - BENPHYSIO, Effective Manual Therapy in Town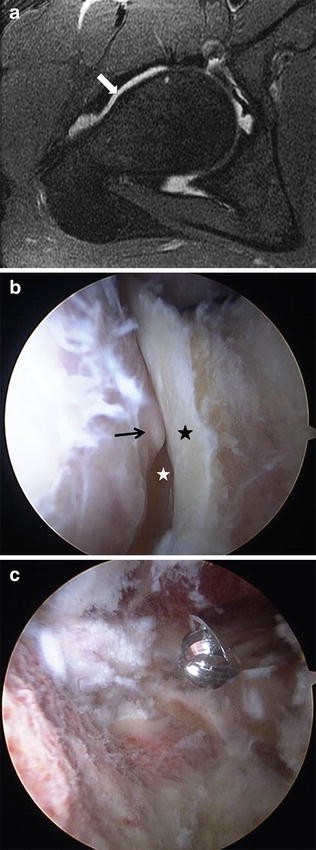
MRI of the Hip: Important Injuries of the Adult Athlete | SpringerLink
When is Hip Arthroscopy an Effective Course of Treatment? - The Leone Center for Orthopedic Care
Imaging of Hip Pain: From Radiography to Cross-Sectional Imaging Techniques
Groin Pain Archives - Benedict Nwachukwu, MD, MBA | Hip, Knee & Shoulder Specialist | Orthopedic Surgeon | Manhattan, Brooklyn, New York City
Groin pain caused by iliopsoas synovial cyst treated with endoscopic approach. A case report
Right Groin Pain in Indians: Causes & How to Prevent It
Gynecological Findings Encountered on Musculoskeletal MRI - Radsource
Hip Labral Tear: Symptoms & Surgery | University of Utah Health
Can A Bad Hip Cause Buttock Pain - Can Ovarian Cyst Cause Hip Pain
:max_bytes(150000):strip_icc()/groinpainfinal-01-5c05dbbdc9e77c00011054d4.png) Groin Pain: Causes, Treatment, and When to See a Doctor
Groin Pain: Causes, Treatment, and When to See a Doctor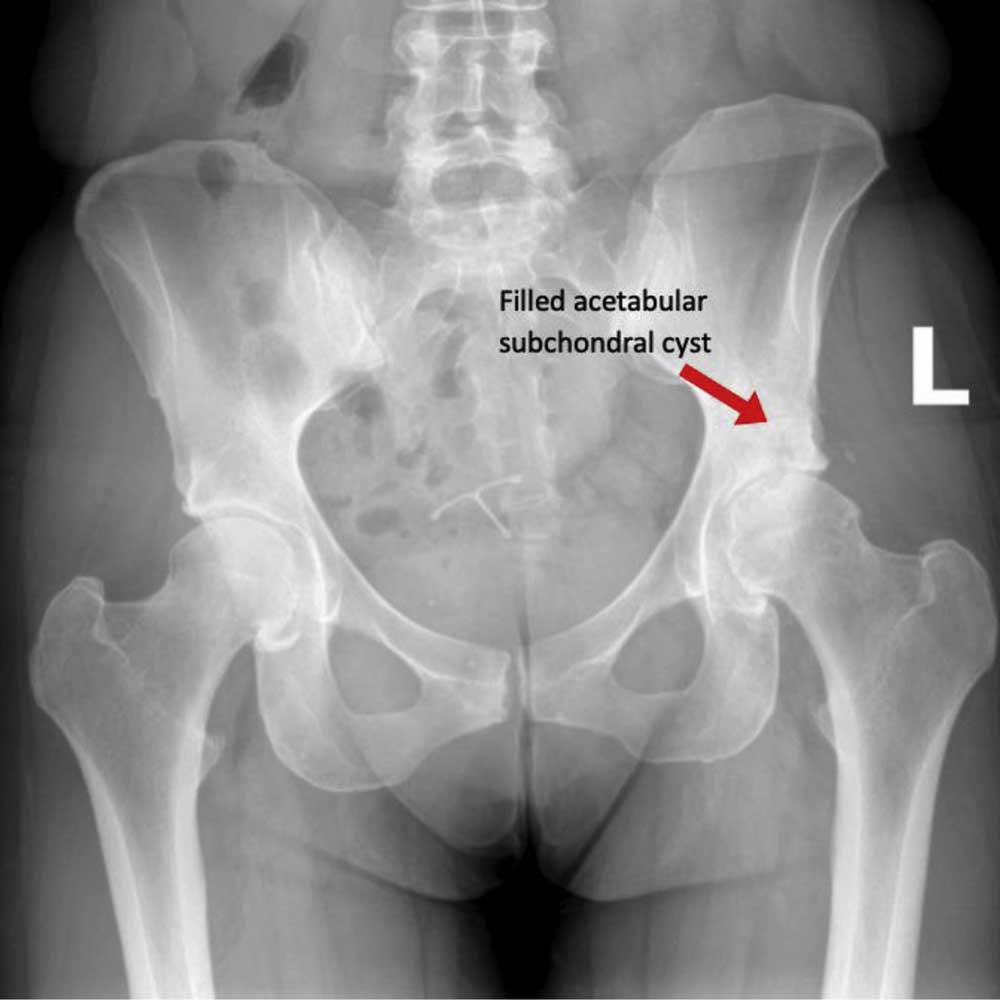





















Posting Komentar untuk "hip cysts and groin pain"